
Leah Croll, MD
With the US Food and Drug Administration's (FDA's) full stamp of approval in hand, Leqembi (lecanemab) is poised to catapult us into a new era of treatment for Alzheimer's disease. And now that the donanemab trial data are out, there's another anti-amyloid drug waiting in the wings.
To finally have true disease-modifying therapies for Alzheimer's disease is a massive step forward for a field that's been plagued with disappointment. But these drugs come with serious concerns and unknowns. They will require complex decision-making, putting doctors, patients, and their families in a medical quandary.
Striking the right balance between cautious optimism and realistic expectations will be a formidable challenge.
Managing Patient and Family Expectations
These drugs are no magic bullet. They slow down the dementia's progression, buying patients more time (on the order of months) before they begin to experience significant worsening. We'll need a lot more information from research and clinical experience before we can understand how meaningful that treatment effect is. Right now, it is unclear whether eligible patients and their families will even perceive tangible differences.
In the CLARITY-AD trial, participants on lecanemab experienced a 27% slowing in the rate of cognitive decline over 18 months. Donanemab was shown to slow decline in memory and cognition by about 35% over the same timeframe in the TRAILBLAZER-ALZ 2 trial. That translates to more time for patients and their families to enjoy independence, maintain normal life, and stave off the most distressing parts of the disease.
But what happens after 18 months of treatment — will the treatment effect magnify or dissipate? How much time are we really buying in the long run? Counseling patients and their families is made all the more difficult when the answers to important questions like these remain to be seen.
Only a Sliver of Alzheimer's Patients Are Current Candidates
The fact is that most patients living with Alzheimer's disease will not qualify for treatment with these drugs. Lecanemab is approved for people with early-stage disease, meaning their dementia is mild or they have mild cognitive impairment, which is a precursor to full-blown Alzheimer's disease. Of the 6 million people in the US living with Alzheimer's, only about 1.5 million are estimated to fall into that category. We can expect to see a similar qualifier for donanemab if it receives FDA approval, especially because that trial suggested a more pronounced treatment effect for patients in the earliest stages of the disease.
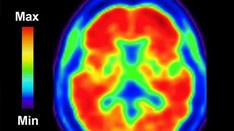
Even if a patient hits the sweet spot where they have just enough cognitive impairment, but not too much, they aren't technically therapeutic candidates until prerequisite testing confirms amyloid protein accumulation in the brain via PET scan or cerebrospinal fluid analysis.
Even then, the FDA's black-box warning for lecanemab recommends that patients undergo genetic testing for the apolipoprotein epsilon 4 (APOE-ε4) mutation to identify those at a particularly high risk for severe adverse effects including brain bleeding and swelling. This recommendation is not unreasonable considering that 15% of the Alzheimer's population has two copies of the APOE ε4 mutation and fall into that high-risk group.
Significant Risks
Anti-amyloid drugs are well-known to cause serious side effects. In the lecanemab trial, 13% of participants receiving Leqembi experienced brain swelling (vs 2% of participants receiving placebo) and 17% of participants had brain bleeding (vs 9% of participants on placebo). In the donanemab trial, brain bleeding occurred in 31.4% of participants on the drug (vs 13.6% on placebo) and swelling occurred in 24% (vs 2.1% receiving placebo). Thankfully, in both trials, most of these adverse events did not produce significant symptoms, but in rare cases these events caused severe or catastrophic neurologic injury, including death.
How can we best guide patients and their families to weigh the uncertain benefits against potentially serious risks? We can start by considering the patient characteristics most likely to portend increased risk for serious side effects: APOE ε4 mutations, blood thinner use, and the presence of microhemorrhages on brain imaging. But after that, we're left with a lot of uncertainty in terms of which patients are most likely to see meaningful clinical improvements from the drug and unknown factors that may increase the risks of treatment.
A Costly Therapy
Medicare plans to cover 80% of lecanemab's steep cost of $26,500 per year. Still, that will leave many patients with a hefty copay, potentially over $6000 per year. But that only scratches the surface. Consider the frequent medical visits, repeated brain scans, laboratory tests, and infusion center appointments. It's been estimated that all-in, the treatment will actually cost about $90,000 per year.
Yes, Medicare will reimburse a large portion of that cost, but it adds up to an estimated $2 billion per year for about 85,000 patients. This will probably spur increases to Medicare premiums, among other economic consequences for the healthcare system.
We'll probably have to wait for an FDA approval decision before we know where donanemab will be priced.
Logistical Challenges Could Be a Rate-Limiting Step
Ask anyone who's tried to see a neurologist recently, and they'll tell you that the wait for a new patient appointment is months long. The shortage of neurologists in the US is already a crisis, and there are even fewer cognitive neurologists. How long will patients be forced to wait for their diagnosis?
Many geriatricians will get comfortable prescribing these drugs, but will our already overburdened primary care providers have the bandwidth to do the same? It's a tall order.
A new world of Alzheimer's treatments also means that the infrastructure of our healthcare systems will need to be ramped up. Lecanemab infusions are administered every 2 weeks and donanemab every 4 weeks. Infusion centers will need to accommodate a lot more patients. And those patients will need frequent brain scans, so neuroimaging centers will need to increase their capacity to perform many more brain MRI and PET scans.
Anti-Amyloid Drugs: An Exciting First Step
The bottom line is that these drugs aren't the Alzheimer's holy grail: an accessible treatment that could stop the disease in its tracks or reverse cognitive impairment. They are, however, a very promising breakthrough.
Yes, there are a ton of kinks to work out here, but this is an exciting start. Alzheimer's research is entering a renaissance era that will hopefully bring more groundbreaking developments. Better biomarkers to facilitate faster, easier diagnosis. More drugs that go beyond amyloid proteins for their therapeutic targets. Treatments for later-stage disease. Drugs that prevent dementia altogether.
Ultimately, these new anti-amyloid beta drugs are an exciting indication that we will eventually have a toolkit of Alzheimer's drugs to choose from. For now, we've taken a solid step forward and there is ample reason to be hopeful for the future.
Leah Croll, MD, is an Assistant Professor of Neurology at the Lewis Katz School of Medicine at Temple University. She completed her neurology residency and stroke fellowship at NYU Langone Health. Aside from clinical practice in stroke neurology, her professional interests include education and medical media. In her free time, she is working on trying all the pastries in Philadelphia, one bakery at a time.
Reach her on Instagram @DrLeahCroll and Twitter @DrLeahCroll
Follow Medscape on Facebook, Twitter, Instagram, and YouTube
Credits:
Lead image: Robert Kneschke/Dreamstime
Image 1: Leah Croll, MD
Medscape Neurology © 2023 WebMD, LLC
Any views expressed above are the author's own and do not necessarily reflect the views of WebMD or Medscape.
Cite this: New Alzheimer's Drugs: Setting Realistic Expectations - Medscape - Jul 25, 2023.











Comments