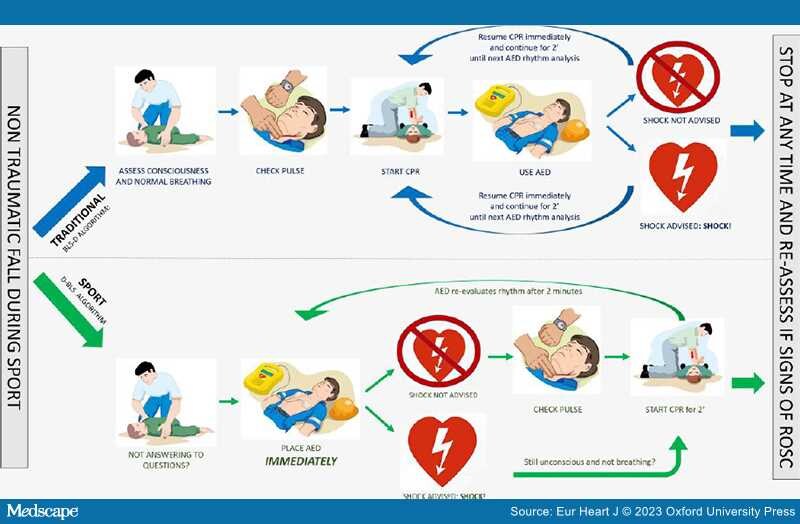
Graphical Abstract
The figure shows a working hypothesis, generated by the results of the meta-analysis of Michelland et al., proposing an adaptation of the standard resuscitation algorithm (BLS-D) to a more specific (and expectedly more effective) protocol for management of sports-related sudden cardiac arrest (D-BLS). According to the proposed protocol, in the case of a witnessed non-traumatic fall during sports activity and an AED available in the field within moments, immediate placement of the device pads and rhythm analysis takes priority over other resuscitation manoeuvres. Accordingly, medical personnel attending sport events could be educated in the following actions: if an athlete falls to the ground and does not respond to questions, even if he/she appears to be breathing or moving, immediately bring the AED, switch it on, place the pads on the chest, and just listen to the voice prompts. If the shock is not advised, start assessment and treatment according to the standard resuscitation algorithm.[8] This working hypothesis needs to be tested by appropriated trials. AED = automated external defibrillator; BLS-D = basic life support and defibrillation; CPR = cardiopulmonary resuscitation; D-BLS = defibrillation and basic life support; ROSC = return of spontaneous circulation.
Although regular sports activity provides substantial health benefits, intense exercise may act as a trigger of sudden cardiac arrest (SCA) and death (SCD).[1] The most common mechanism of SCD during sports activity is abrupt, adrenergic-dependent ventricular fibrillation (VF) as a consequence of an underlying clinically silent cardiovascular disorder. The cause of SCD reflects the age of participants: while in middle-aged/senior athletes atherosclerotic coronary artery disease accounts for the vast majority of fatal events, in young competitive athletes (age ≤35 years) there is a broad spectrum of pathological substrates consisting of genetic heart muscle diseases, such as hypertrophic cardiomyopathy and arrhythmogenic right ventricular cardiomyopathy, followed by congenital anomalies of coronary arteries, aortic rupture in Marfan's syndrome, myocarditis (either acute myocardial inflammation or post-inflammatory myocardial scar), and valvular diseases, including aortic valve stenosis and mitral valve prolapse. A sizeable proportion of athletes experiencing SCA have no evidence of structural heart disease, and the cause of the electrical ventricular instability is a primary electrical cardiac condition, namely either inherited cardiac ion channel defects (channelopathies) including long QT syndrome, catecholaminergic polymorphic ventricular tachycardia, and Brugada syndrome, or idiopathic ventricular fibrillation.[2]
The SCD of an athlete is a rare event, but its catastrophic nature mandates the medical community to develop and implement effective preventive strategies. Screening before participation in sports has the potential to reduce the risk of SCD by the early (at pre-symptomatic stage) identification of athletes affected by heart diseases.[3] However, screening lacks sensitivity for detection of cardiac conditions such as atherosclerotic coronary artery disease or congenital anomalies of coronary arteries, that usually do not manifest with abnormalities on basal 12-lead ECG. Recent clinical and pathological studies have demonstrated that a non-ischaemic left ventricular myocardial scar may be a not so uncommon and clinically concealed substrate of life-threatening arrhythmias in the athlete.[4] This myocardial lesion may be caused by a variety of myocardial diseases, including myocarditis, sarcoidosis, and genetic cardiomyopathies. Although non-ischaemic left ventricular scar is a potential source of effort-induced ventricular arrhythmias detectable by exercise testing and/or Holter monitoring, the diagnostic power of standard ECG is limited because suspicious abnormalities such as low QRS voltages in limb leads and T-wave inversion in lateral leads are found in a minority of affected patients. Moreover, the segmental nature of the left ventricular myocardial scar involving the epicardial–mid-myocardial wall layers, but sparing the subendocardium, which contributes most to myocardial thickening, explains why it is usually missed by echocardiography and only evidenced as late gadolinium enhancement on cardiac magnetic resonance. The difficulty in identifying affected athletes by routine pre-participation ECG screening makes this condition one of the most challenging and unpredictable causes of SCD during sports.[4,5]
These screening limitations justify the increasing efforts for implementing cardiopulmonary resuscitation intervention programmes including an automated external defibrillator (AED) for treating arrhythmic SCA in the athletic field. Several studies demonstrated that immediate cardiopulmonary resuscitation (CPR) manoeuvres and the use of on-site AED providing early defibrillation play a pivotal role in reducing mortality and post-anoxic brain damage in sport-induced SCA victims.[6] The evidence that early shock is life saving makes the terms 'cardiac arrest' and 'sudden death' in the athlete fortunately no longer interchangeable, with SCA being a treatable event. In contrast to the past tragic events of professional football players, such as Marc Vivian Foe, Antonio Puerta, and Pier Mario Morosini who did not survive SCA on the pitch, the recent good outcome of the football player Christian Eriksen and the cyclist Sonny Colbrelli are emblematic of the extraordinary advances in the last years of successful treatment of SCA occurring during sports activity.[5]
In this issue of the European Heart Journal, a systematic review and meta-analysis by Michelland et al.[7] provides robust data on the favourable impact of basic life support-defibrillation (BLS-D) on survival in sports-related SCA. Bystander presence, bystander CPR, and bystander use of an AED improved the survival without neurological damage. The study confirms and extends the results of previous investigations showing the success of the emergency response in the case of sports-related SCA based on quick recognition, timely CPR, and early defibrillation, which represent the main steps of the so-called 'chain of survival' in the established BLS-D protocols.[8] Most importantly, the use of an AED had the greatest impact on survival [odds ratio (OR) = 5.25], compared with bystander presence (OR = 2.55) and bystander CPR (OR = 3.84). This finding may be related to the high proportion of shockable rhythm, which was documented in three-quarters of SCAs during sport. This rate is greater than that reported in the general population of non-athletes experiencing out-of-hospital cardiac arrest, which has been estimated at <50% and reported to further decline worldwide.[9] This may be explained by the aetiology of SCA during sports, which predominantly includes substrates such as acute coronary syndrome, cardiomyopathies, or myocarditis, predisposing to adrenergic-dependent ventricular fibrillation that can be successfully treated by early defibrillation.[2] Of importance, the benefits on survival of both bystander CPR and AED were observed in both competitive/professional and leisure time groups. The implication of this finding is that a proper emergency response planning with immediate access to an AED represents an emerging task (with problems of feasibility, logistics, and costs) for prevention of SCD of the growing number of subjects, mostly middle/aged and senior, engaged in recreational sports activity outside the community of competitive/professional athletes.[3]
Among the study limitations, it should be stressed that there is a lack of information regarding the quality of CPR, the first recorded rhythm, and the number of delivered shocks, all recognized factors which may affect the prognosis of out-of-hospital cardiac arrest.
The meta-analysis by Michelland et al.[7] provides 'shocking' insights into the impact of BLS-D on survival after exercise-related SCA and offers the potential to generate working hypotheses for improving the survival algorithm of the management of SCA in athletes, which is an event characteristically witnessed and with immediate access to on-site AED, both conditions providing the unique opportunity of rapid resuscitation by early defibrillation. The time between the athlete's collapse and the recognition of SCA prompting early defibrillation is critical to survival without any neurological consequences. Of note, ischaemic brain injury after cardiac arrest is an important predictor of short-term mortality but also a major determinant of the long-term prognosis and quality of life in survivors of out-of-hospital cardiac arrest. A poor neurological outcome may lead to cognitive impairment, restricted mobility, depression, or even vegetative state.[10]
The review of SCA during sports activity recorded on video shows that many cases received late and suboptimal resuscitation even when the medical team equipped with an AED was on the sideline.[11–13] Watching these videos may help to understand the reasons for the delayed recognition of SCA, that include a series of factors such as the reaction slowed down by the stupor due to the unexpected event, the time-consuming attempt to open the airway and prevent 'tongue swallowing', and the misinterpretation of agonal breathing and involuntary limb movements.[14] Because early defibrillation has become the crucial step in the life support algorithm, bystander(s) should not hesitate to use the on-site AED to immediately interrupt ventricular fibrillation and restore the normal electrical activity of the heart. The availability of an AED in the field allows the step of SCA recognition, which represents a critical obstacle to prompt an athlete's resuscitation, to be skipped. Indeed, AEDs are highly reliable tools which analyse the heart rhythm and prompt rescuers to only deliver a shock in the case of ventricular fibrillation or ventricular tachycardia, which are responsible for the vast majority of SCAs during sport, as confirmed by the study of Michelland et al.[7] Besides providing life-saving shocks, the majority of AEDs guide rescuers with voice and visual instructions through the different phases of resuscitation. As the automatic rhythm analysis takes only a few seconds, immediate AED placement in any case of non-traumatic fall when the athlete does not respond to questions, avoiding waste of time for breathing and pulse assessment, is likely to further increase the chance of survival without neurological consequences. We propose as a working hypothesis to adapt the standard resuscitation algorithm to a more specific (and expectedly more effective) protocol for management of sports-related cardiac arrest, with the aim to benefit most from the immediate defibrillation using the in-the-field AED (Graphical Abstract).
In conclusion, sport-related SCA is characteristically witnessed, providing the opportunity for rapid CPR and prompt access to on-site AED which result in excellent rates of survival, as shown by the study of Michelland et al.[7] However, still today athletes experiencing witnessed SCA may die or have severe cerebral damage because cardiac arrest is not promptly recognized and defibrillation is too late. Since most SCAs during sports are shockable and early defibrillation critically influences the outcome, further improvement of survival is expected by immediate use of the AED in the case of a non-traumatic fall of an athlete, skipping traditional steps of the resuscitation protocol, such as time-consuming recognition of cardiac arrest, and letting the device do the job first. This working hypothesis needs to be tested by further studies. Implementation of emergency programmes for prevention of SCD in athletes is warranted, with widespread distribution of AEDs in sports arenas and training of coaches and staff to perform resuscitation intervention with early defibrillation.
Eur Heart J. 2023;44(3):193-195. © 2023 Oxford University Press
Copyright 2007 European Society of Cardiology. Published by Oxford University Press. All rights reserved.