Find the latest COVID-19 news and guidance in Medscape's Coronavirus Resource Center.
A Possible Complication of COVID-19?
A 75-year-old woman with a history of type 2 diabetes and hypertension presents to the emergency department with worsening dyspnea, productive cough, and diarrhea for 10 days. Six days earlier, she had a positive test for SARS-CoV-2 and was prescribed doxycycline and hydroxychloroquine. In the emergency department, blood and sputum cultures are obtained and she is begun on vancomycin and cefepime as empirical treatment for a possible secondary bacterial infection.
Physical examination:
Temperature: 99°F (37.2°C)
Heart rate: 69 beats/min
Respiratory rate: 24 breaths/min
Blood pressure: 167/52 mm Hg
Oxygen saturation: 89% on 2 L nasal cannula
General examination: Appears fully alert but is mildly tachypneic, with mildly increased work of breathing.
Chest examination: Clear to auscultation bilaterally, without rhonchi or rales.
Other systems: Examination of the cardiovascular, gastrointestinal, and neurologic systems and the head and skin were unremarkable.
Laboratory findings on admission:
Leukopenia (white blood cell count 2.8 cells/µL), including lymphopenia (14%)
Renal impairment (blood urea nitrogen level 52 mg/dL, creatinine level 1.9 mg/dL, estimated glomerular filtration rate 26 mL/min/1.73 m2)
Sputum cultures: Pseudomonas aeruginosa
Blood cultures: Negative (on admission and 5, 10, and 14 days after admission)
HIV negative
Source: Peter Pappas, MD, Division of Infectious Diseases, University of Alabama at Birmingham
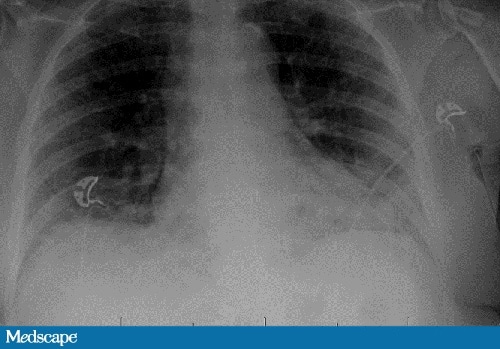
Chest radiography: Basilar atelectasis and basilar predominant airspace disease, concerning for multifocal infection in the setting of known atypical viral infection.
Chest CT: Multilobar bilateral pulmonary ground-glass opacities compatible with history of COVID pneumonia.
Hospital Course: Day 2
The patient develops worsening hypoxia in the absence of fever and is transferred to the intensive care unit (ICU), where she is intubated. She is started on remdesivir and dexamethasone.
Over the next week, the patient's oxygen requirement continues to increase, and she develops a fever despite broad-spectrum antibacterial medications and negative blood, sputum, and urine bacterial cultures. Fungal infection is suspected.
Cite this: The COVID Complication You Might Miss - Medscape - Nov 19, 2020.