Insulin costs have skyrocketed, meaning that more and more patients are unable to afford analogue preparations and must return to the bad old days of using human insulins in a vial rather than preloaded pens. While there are definitely downsides to the switch, at least one study conducted in a Medicare population provides reassurance to clinicians and patients that the switch can be done without a loss of control.
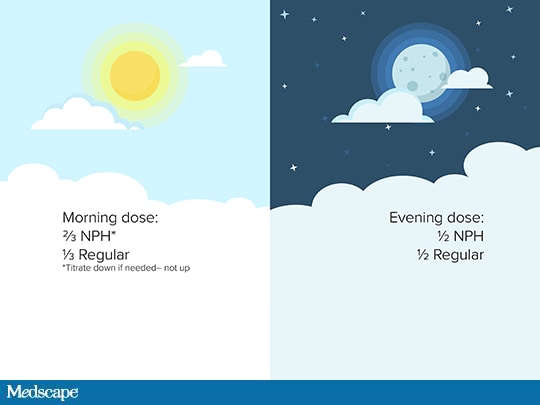
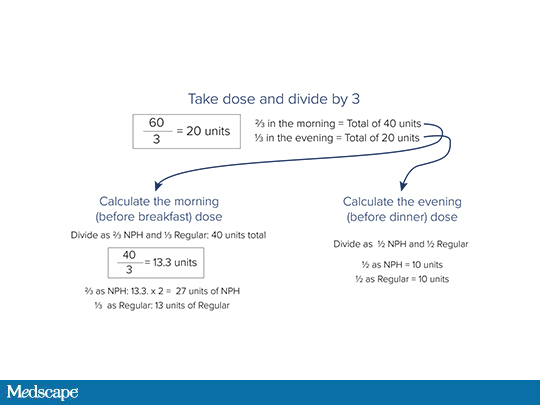
What are the basic steps in switching a patient from an analogue insulin to a split mixed human insulin regimen? Dr Jay Shubrook walks us through the math.
Medscape Family Medicine © 2019 WebMD, LLC
Any views expressed above are the author's own and do not necessarily reflect the views of WebMD or Medscape.
Cite this: Doing the Math: Converting Analogue to Human Insulin - Medscape - Jun 12, 2019.













Comments